dislocated shoulder exercises pdf
Rehabilitation after a shoulder dislocation aims to safely restore function. This process involves a structured program, often spanning several months. It focuses on regaining range of motion, strength, and stability following an anterior shoulder dislocation, a common injury. The rehabilitation program may be modified based on individual needs.
Understanding Anterior Shoulder Dislocation
Anterior shoulder dislocation occurs when the upper arm bone pops out of the shoulder socket, usually forward. This is often caused by trauma, like a fall or sports injury. Understanding the mechanism of this injury is crucial for effective rehabilitation. The shoulder joint relies on ligaments, muscles, and tendons for stability. When dislocated, these structures can be stretched or torn, leading to pain, instability, and limited movement. Rehabilitation programs are designed to address these specific issues. The goal is to restore the dynamic joint stability, focusing on muscle strengthening and proprioception. This approach helps prevent future dislocations and facilitates a safe return to activity. The initial phase may involve a period of immobilization and then proceed to gentle exercises.
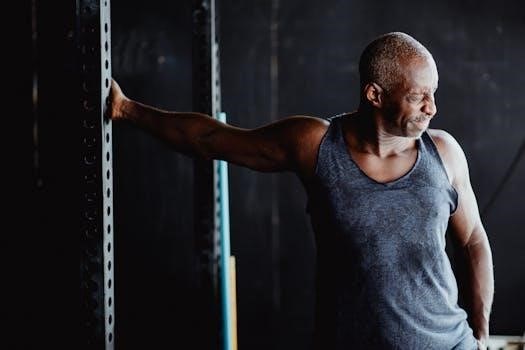
Rehabilitation Phases Overview
Rehabilitation is typically structured into three phases. These phases gradually increase the intensity of exercises. They are designed to restore movement, build strength, and return to full activity, while ensuring safe progression.
Phase One⁚ Initial Recovery (0-4 Weeks)
The initial recovery phase, typically spanning 0 to 4 weeks, focuses on pain management and gentle restoration of range of motion. During this period, the primary goal is to allow the injured tissues to heal while minimizing further stress on the anterior joint capsule. Activities will usually include the use of a sling for comfort, and it is recommended to wean off this as comfortable. Gentle exercises, such as pendulum exercises, are introduced. These exercises help to maintain some movement without putting undue strain on the shoulder. It is important to avoid any movements that could cause pain or discomfort. Scapular setting exercises may also be included to maintain proper shoulder blade position. Physical therapy can begin immediately for recurrent dislocators, and for first-time dislocators, immobilization may be used for 3-4 weeks before starting therapy. The focus is on establishing movement and reducing pain, with a slow and cautious approach.
Phase Two⁚ Strengthening and Stability (4-12 Weeks)
Phase two, typically occurring between 4 to 12 weeks, focuses on building strength and stability in the shoulder joint. During this stage, exercises will progress to include strengthening of the rotator cuff muscles and scapular stabilizers. Emphasis will be on controlled movements to avoid placing undue stress on the anterior joint capsule. Proprioceptive exercises are introduced to improve joint awareness. The goal is to restore dynamic joint stability, allowing the shoulder to handle more activity. Exercises might include gentle resistance work, progressing slowly as tolerated, to ensure the shoulder is stable. The focus remains on safety and controlled movement, ensuring the shoulder is ready for higher levels of activity. This phase is crucial for preparing the shoulder for a return to functional use and more demanding movements, ensuring a full recovery. Individuals may begin to overlap phases one and two depending on their progress.
Phase Three⁚ Return to Activity (12+ Weeks)
Phase three, beginning at 12 weeks and beyond, concentrates on a safe return to full activity. The primary aim is to integrate the shoulder back into functional movements and sport-specific tasks. This phase focuses on regaining full strength, power, and endurance. Exercises advance to include more dynamic and challenging activities, carefully monitored to prevent re-injury. Individuals may gradually resume sport-specific training, with attention to proper technique. The emphasis is on ensuring the shoulder can handle the demands of daily life and desired activities. This phase often involves advanced proprioceptive exercises and plyometric drills. The return to full activity is gradual, and the individual should continue to monitor for any signs of discomfort. Individuals may overlap phases two and three, depending on progress. This phase is vital for achieving a complete recovery, allowing individuals to return to their desired activities confidently.

Key Exercise Types
Rehabilitation includes specific exercises for recovery. These exercises aim to improve strength and stability. Pendulum, scapular setting, and proprioceptive exercises are commonly used to help restore shoulder function after a dislocation.
Pendulum Exercises
Pendulum exercises are a gentle way to begin shoulder rehabilitation after a dislocation. These exercises help to restore range of motion without putting excessive stress on the joint. To perform them, stand and lean forward, supporting yourself with your non-injured arm. Allow your injured arm to hang down freely. Gently swing your arm forward and backward, then side to side, and finally in small circles. Start slowly and gradually increase the range of motion as you feel comfortable. It’s crucial to relax your shoulder muscles and let the momentum of your arm do the work. These exercises help to improve circulation, reduce stiffness, and promote healing during the initial recovery phase. These are typically performed in the early stages of rehab.
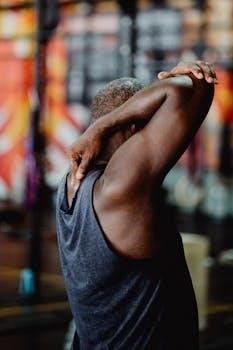
Scapular Setting Exercises
Scapular setting exercises are important for restoring stability and proper movement in the shoulder after a dislocation. These exercises focus on controlling the shoulder blade, or scapula, which plays a crucial role in overall shoulder function. To perform a scapular setting exercise, start by standing or sitting with good posture. Gently squeeze your shoulder blades together, as if trying to hold a pencil between them, then relax. Avoid shrugging your shoulders or arching your back. You should feel a slight activation of the muscles between your shoulder blades. These exercises improve scapular control, which is essential for stabilizing the shoulder joint and preventing future dislocations. They also help to engage core muscles, which support the shoulder during movements. Consistent practice of these exercises contributes to long-term stability and function.
Proprioceptive Exercises
Proprioceptive exercises play a vital role in restoring balance and awareness of the shoulder joint after a dislocation. These exercises focus on improving the body’s ability to sense its position and movement in space, known as proprioception. Examples of proprioceptive exercises include weight shifting, reaching activities, and working with unstable surfaces. These activities help to retrain the nervous system to better control and stabilize the shoulder joint. These should start with simple movements and gradually increase in complexity as the shoulder strengthens. Using tools such as balance boards or wobble cushions can add to the challenge and effectiveness of proprioceptive training. Performing these exercises regularly will improve your ability to react to changes in position, enhancing stability and reducing the risk of re-injury. These exercises are crucial for a full recovery.
Rehabilitation Protocols
Rehabilitation protocols guide the recovery process following a shoulder dislocation. These protocols outline specific phases and exercises tailored to different stages of healing. They often vary depending on surgical or non-surgical intervention.
Non-Operative Rehabilitation Protocol
The non-operative rehabilitation protocol for a dislocated shoulder is a structured approach designed to restore function without surgery. This protocol typically begins with a period of immobilization, often using a sling, for several weeks, especially for first-time dislocators. Following immobilization, physical therapy begins to focus on regaining full range of motion, and pain management. The exercises start gently to avoid undue stress on the anterior joint capsule. The program progresses through phases, gradually increasing the intensity of exercises to strengthen the shoulder muscles. Proprioceptive exercises are also included to enhance joint stability. The time in each phase will be adjusted based on individual progress. It’s a progressive process, aiming to return individuals to their desired activities as safely as possible. Regular assessment by a physical therapist helps to tailor the protocol to each individual’s needs and healing progress.
Post-Surgical Rehabilitation Considerations
Post-surgical rehabilitation after a shoulder dislocation requires a tailored approach. Initial phases often emphasize protecting the surgical repair and minimizing pain. Immobilization with a sling is often necessary to allow for proper healing. The rehab program focuses on regaining range of motion gradually, following the surgeon’s specific instructions. Strengthening exercises are introduced later, after sufficient healing has occurred, targeting the muscles surrounding the shoulder joint. Proprioceptive exercises form an essential part of the program to regain joint stability and control. Progression through each phase is carefully monitored and adjusted based on the individual’s healing and progress. A collaborative approach with the surgeon and physical therapist is crucial. The timeline may be longer than non-operative rehabilitation, and the patient must adhere to the guidelines to ensure optimal outcomes. Careful attention is paid to preventing reinjury.

Important Considerations
Individualized treatment plans are essential for successful rehabilitation. Progression should be based on specific criteria, and seeking professional guidance is vital. The rehabilitation duration may vary greatly, depending on multiple factors.
Individualized Treatment Plans
Rehabilitation protocols for a dislocated shoulder should always be tailored to the individual. Factors such as the severity of the dislocation, the patient’s age, activity level, and any prior shoulder issues must be considered. A first-time dislocator might have a different rehabilitation path compared to someone with recurrent dislocations. Furthermore, the presence of any associated injuries, such as labral tears or rotator cuff issues, will impact the rehabilitation process. The surgeon’s specific recommendations and any deviations from standard protocols must also be incorporated. Physical therapy evaluations should guide the plan, ensuring it aligns with the patient’s specific needs and goals. Close monitoring is essential to adjust the plan as needed, optimizing recovery and minimizing the risk of re-injury. This involves careful observation of the patient’s response to exercises and activities, with adjustments made to the intensity and type of exercise. The plan should be progressive, moving forward based on the patient’s tolerance.
Progression Criteria
Advancement through the rehabilitation phases after a shoulder dislocation is based on meeting specific criteria. These criteria ensure a safe and effective return to activity. Initially, the focus is on pain management and achieving a full range of motion without discomfort. Once pain is controlled and motion is restored, the patient can progress to strengthening exercises. Criteria for advancing to the next phase might include consistent performance of exercises with good form, minimal pain, and no signs of inflammation. It is crucial that the patient demonstrates sufficient strength and stability before progressing to more challenging activities. The ability to control the shoulder throughout the range of motion is also a key indicator. Progression should not be based solely on time but rather on the individual’s response to the treatment. There should be no signs of re-injury or instability before moving forward. Regular assessment by a physical therapist is critical to assess progress and adjust the program accordingly.
When to Seek Professional Guidance
Seeking professional guidance after a shoulder dislocation is crucial for optimal recovery. It’s essential to consult a physical therapist or physician if pain increases or if range of motion decreases. Any signs of instability, such as the shoulder feeling like it might dislocate again, should be addressed promptly. If you experience numbness, tingling, or weakness in the arm or hand, seek immediate medical attention. These could indicate nerve involvement. If you’re unsure about the proper technique for exercises or if you’re not progressing as expected, a healthcare professional can provide valuable feedback. They can also adjust the program to meet your specific needs. Don’t hesitate to seek guidance if you have any questions about your rehabilitation protocol. Professional guidance is essential for ensuring a safe and effective rehabilitation process. It can also help to prevent re-injury and ensure optimal function of the shoulder joint.